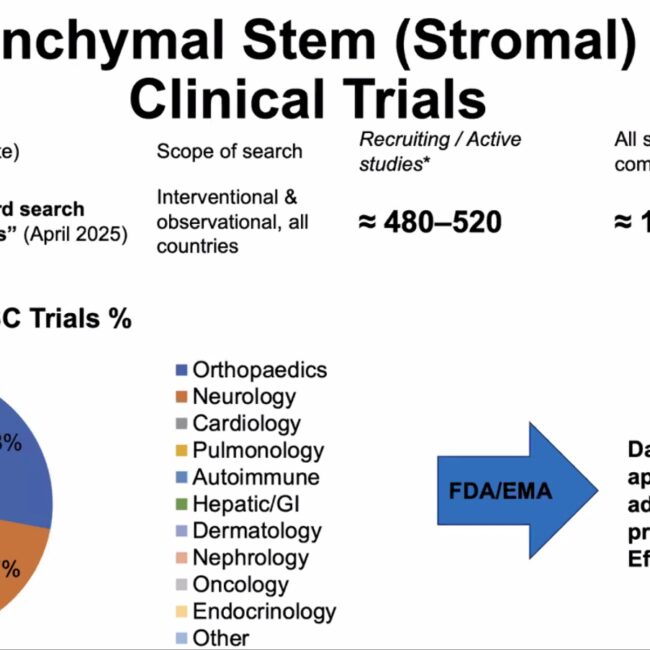
THE FUTURE OF HEALTH IS IN BIOLOGY
🦴 Regenerative Medicine in Orthopedics: A New Era of Healing with Stem Cells
🧬 Introduction: From Repair to Regeneration
Traditional orthopedic treatments often focus on managing symptoms or repairing damage. Regenerative medicine, powered by stem cell therapy, represents a breakthrough — aiming to heal damaged tissue at a biological level.
“We are no longer just repairing — we are regenerating.”
📌 What Are Stem Cells?
Stem cells are unique, undifferentiated cells that can transform into specialized musculoskeletal cells (such as bone, cartilage, tendon, or muscle) and stimulate the body’s natural repair mechanisms.
Two key mechanisms:
- Differentiation: Stem cells become the needed tissue (e.g., cartilage).
- Paracrine effect: Stem cells secrete molecules that trigger the body’s own healing response.
Regenerative medicine
- High-quality illustration of stem cell differentiation and paracrine signaling.
- Caption: “Stem cells act as both architects and foremen of tissue repair.”
🩺 Sources of Stem Cells Used in Orthopedics
| Source | Type of Cells | Main Applications | Advantages |
| Bone marrow | Mesenchymal stem cells (MSCs) | Cartilage, tendon, bone regeneration | Autologous, high MSC concentration |
| Adipose tissue (fat) | Adipose-derived regenerative cells (ADRCs) | OA, tendon repair | Abundant, minimally invasive harvest |
| Umbilical cord tissue | Allogenic MSCs | OA, soft tissue injury, advanced cases | High regenerative potential, off-the-shelf availability |
| Platelet-rich plasma (PRP) | Platelet-derived growth factors | Tendinopathies, early OA | Easy harvest, boosts healing environment |
🧪 How Stem Cell Therapy Works
- Harvesting – Bone marrow or adipose tissue (if autologous), or ready-to-use cord MSCs (if allogenic).
- Processing – Isolation, concentration, or expansion according to clinical protocol and regulations.
- Targeted Injection – Image-guided delivery into injured joint, tendon, or bone.
- Regeneration & Remodeling – Modulation of inflammation, stimulation of healing, and tissue regeneration.
- Step-by-step visual or animation of harvesting, processing, injection, and regeneration.
⚕️ Clinical Indications for Stem Cell Therapy in Orthopedics
Stem cell therapy is increasingly used in:
- ✅ Osteoarthritis (knee, hip, shoulder, ankle)
- ✅ Tendon injuries (e.g., rotator cuff, patellar, Achilles)
- ✅ Ligament injuries (e.g., partial ACL tears)
- ✅ Cartilage defects in athletes and active individuals
- ✅ Bone non-union and defects
- ✅ Sports injuries to accelerate healing
🏃 For many patients, this can postpone or avoid major surgery like joint replacement.
📚 Evidence-Based Benefits
- 🔸 Pain reduction through inflammation control
- 🔸 Improved mobility and function
- 🔸 Cartilage regeneration confirmed in MRI studies
- 🔸 Minimally invasive — fast recovery time
- 🔸 Excellent safety profile
🧾 Key Scientific Studies
- Wang et al., 2016 — UC-MSC in knee OA: significant improvement in pain and function.
- Samara et al., 2022 — MRI-documented cartilage regeneration post UC-MSC injection.
- Jo et al., 2018 — Adipose MSC improved tendon healing in rotator cuff disease.
🧠 Safety and Regulatory Considerations
- ✅ Performed under sterile, GMP-compliant conditions.
- 🩺 Only by licensed and trained physicians.
- 📜 Follow local regulatory guidelines (e.g., DHA, EMA, FDA).
- 📝 Patient selection and consent are essential.
🆚 Stem Cell Therapy vs Conventional Treatment
| Conventional Orthopedic Care | Regenerative Stem Cell Therapy |
| Symptom management | Biological regeneration of tissue |
| Often requires surgery | Minimally invasive injection |
| Short-term relief | Potential for long-term healing |
| No regenerative capacity | Stimulates natural repair |
👨⚕️ Who Can Benefit Most?
- Patients with early to moderate osteoarthritis
- Active individuals or athletes with tendon/ligament injuries
- Patients seeking non-surgical options
- Individuals looking for faster recovery with lower downtime
❗ Advanced bone-on-bone arthritis may still require joint replacement.
🚀 Future of Regenerative Orthopedics
- Exosomes & biologics for enhanced healing signals
- Gene-edited stem cells for stronger regenerative potential
- 3D bioprinting for cartilage and bone reconstruction
- AI-driven personalized protocols to predict outcomes

- Futuristic concept illustration of bioprinting or precision medicine.
📝 Conclusion: Healing Reimagined
Stem cell therapy in orthopedics is a game changer.
It focuses not only on relieving pain but on regenerating tissue — restoring mobility, delaying surgery, and improving quality of life.
🌿 Regenerative medicine is not the future — it’s already transforming orthopedic care today.
📚 References
- Wang L. et al., Curative effect of human umbilical cord mesenchymal stem cells by intra-articular injection for degenerative knee osteoarthritis, 2016.
- Samara E. et al., Ultrasound-guided intra-articular injection of expanded umbilical cord mesenchymal stem cells in knee OA, Regen Med, 2022.
- Jo C.H. et al., Intradermal injection of autologous adipose-derived MSCs for rotator cuff disease, Stem Cells, 2018.
- Caplan A.I., Mesenchymal Stem Cells: Time to Change the Name!, Stem Cells Transl Med, 2017.
If you are experiencing joint pain, tendon injury, or early osteoarthritis, regenerative stem cell therapy may offer a minimally invasive, scientifically proven solution.
👉 Book a consultation today with our orthopedic and regenerative medicine specialists.