PRP FOR ATHLETE IMPROVEMENT
🩸 Regenerative Medicine and Orthobiology: PRP Therapy in Modern Orthopedics
🦴 What Is Orthobiology?
Orthobiology is a branch of orthopedic medicine that uses the body’s natural healing mechanisms to accelerate tissue repair and regeneration.
Instead of replacing damaged tissues surgically, orthobiologic treatments aim to stimulate biological healing using:
- 🩸 Platelet-Rich Plasma (PRP)
- 🧬 Stem cells (adipose, bone marrow, umbilical cord)
- 💉 Growth factors and biologic adjuncts (e.g., exosomes, peptides)
Orthobiology blends cutting-edge science with the body’s innate capacity to heal itself — offering patients minimally invasive, safe, and effective solutions.
- Illustration showing the orthobiologic triangle: PRP, stem cells, growth factors.
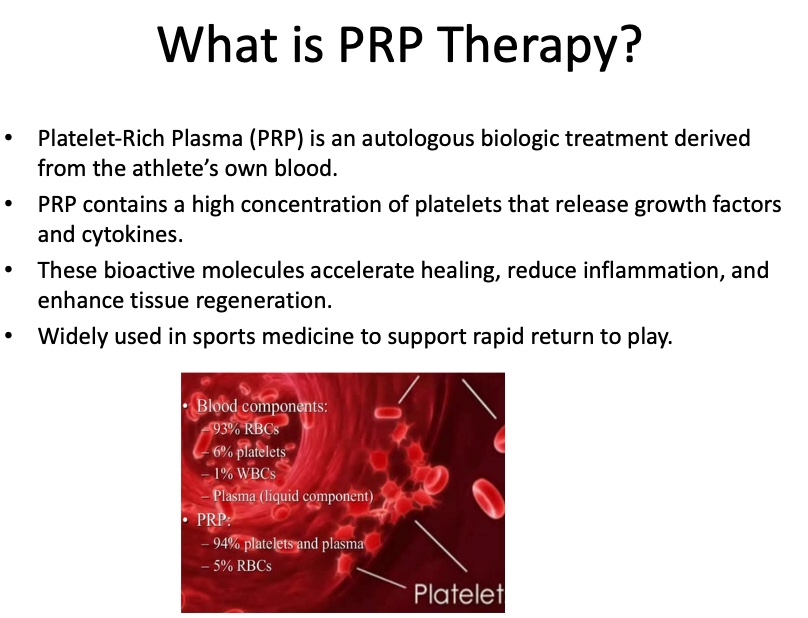
🧬 What Is PRP Therapy?
Platelet-Rich Plasma (PRP) is an autologous (from the patient’s own blood) concentrate of platelets and growth factors.
- Blood is drawn from the patient.
- It is processed via centrifugation to concentrate platelets.
- The PRP is then injected directly into the injured area.
Platelets release bioactive molecules such as PDGF, TGF-β, VEGF, and IGF — powerful mediators that:
- Stimulate cell proliferation and differentiation
- Promote angiogenesis (new blood vessel formation)
- Enhance tendon, cartilage, and bone healing
- Modulate inflammation naturally
PRP is considered the first-line orthobiologic therapy in regenerative orthopedics.
- Diagram of PRP preparation and injection.
💪 PRP Applications in Orthopedics
PRP therapy is widely used in sports medicine, orthopedic surgery, and rehabilitation.
It is particularly effective for:
| Condition | How PRP Helps |
| Tendinopathies (tennis elbow, Achilles) | Stimulates tendon healing, reduces pain |
| Rotator cuff tendinopathy / partial tears | Promotes collagen synthesis and tissue regeneration |
| Osteoarthritis (knee, shoulder, ankle) | Reduces inflammation, improves lubrication, protects cartilage |
| Ligament injuries | Speeds up healing, improves stability |
| Muscle injuries | Shortens recovery time |
| Post-surgical augmentation | Enhances biological healing after orthopedic surgery |
PRP can be used alone or in combination with stem cell therapy for enhanced regenerative effect.
- Anatomy illustration of common PRP targets: knee, shoulder, Achilles tendon.
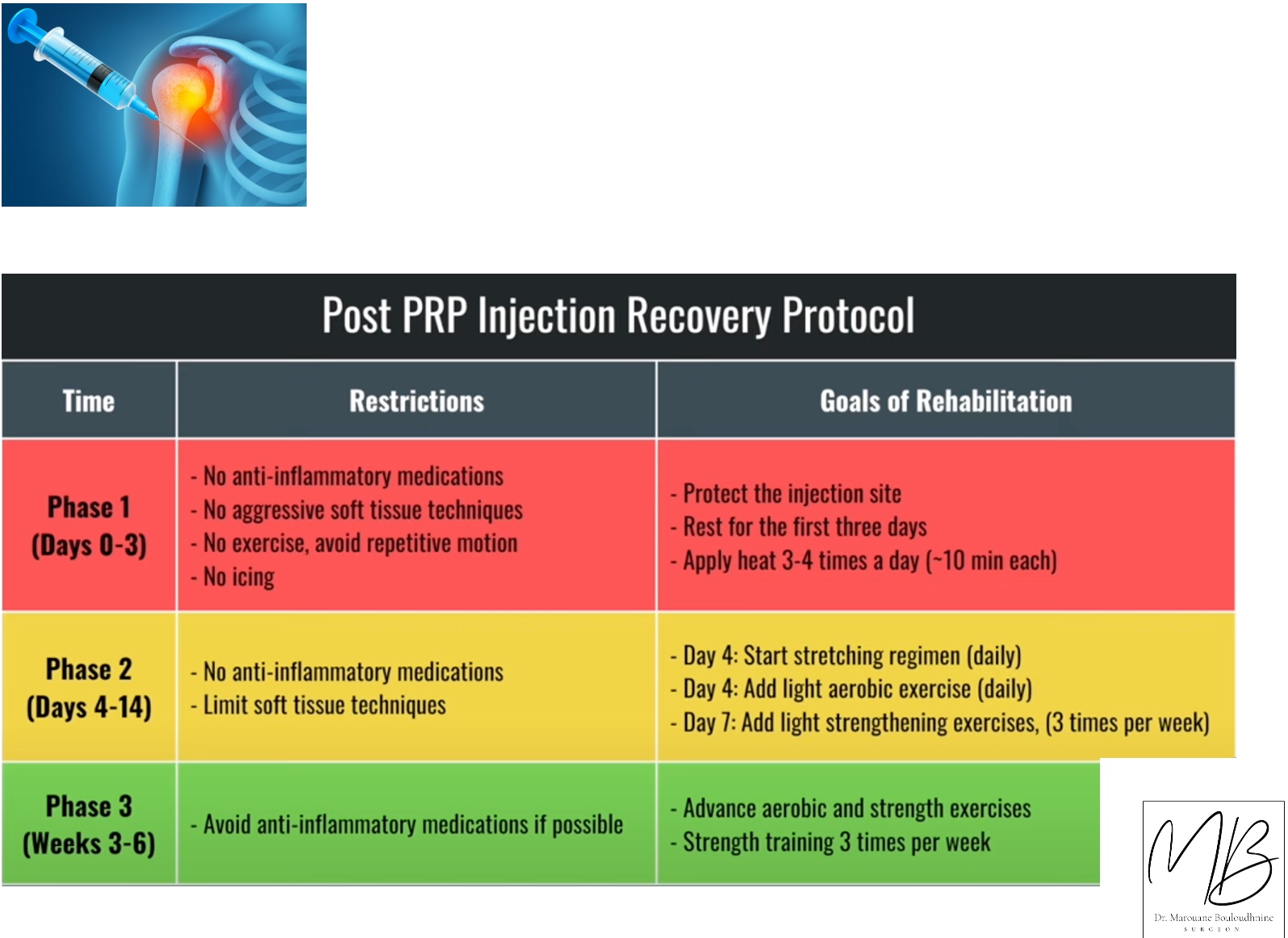
🩻 How the Procedure Works
- Assessment – Physical examination and imaging (ultrasound, MRI) to identify pathology.
- PRP Preparation – Blood is collected and processed under sterile conditions.
- Injection – PRP is delivered under ultrasound or fluoroscopic guidance to the target tissue.
- Recovery – Minimal downtime; rehabilitation may start quickly.
- Regeneration Phase – Biological activity peaks over weeks to months.
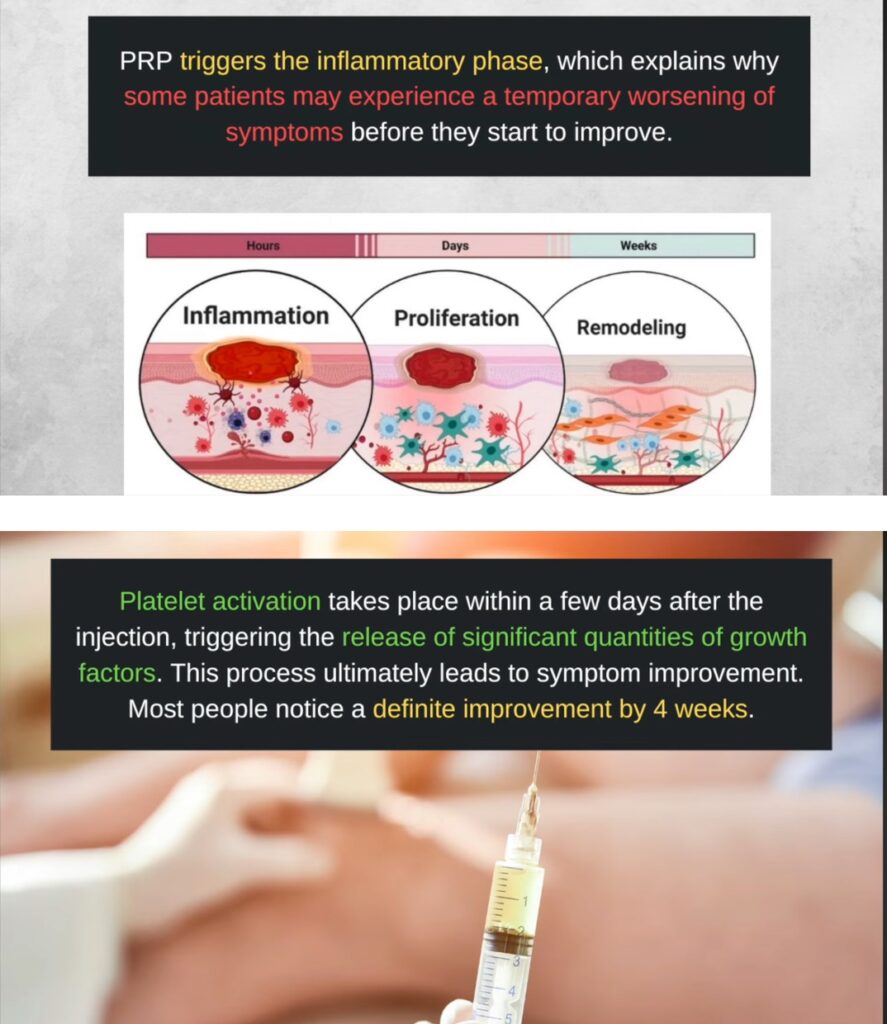
Typical timeline:
- Day 0 → Injection
- Week 1–2 → Initial pain improvement, inflammation control
- Week 4–8 → Collagen remodeling, tissue repair
- Month 3+ → Functional improvement and symptom relief
🧪 Scientific Evidence Supporting PRP
Numerous studies and systematic reviews demonstrate PRP’s efficacy:
- Filardo et al., 2012 — PRP improved pain and function in knee osteoarthritis better than hyaluronic acid.
- Mishra et al., 2014 — PRP was superior to corticosteroids in chronic tennis elbow.
- Samara et al., 2022 — Combined PRP + MSC therapy accelerated cartilage repair in degenerative OA.
- Jo et al., 2018 — PRP enhanced tendon healing response when combined with MSC in rotator cuff disease.
Key Advantages of PRP Therapy:
- ✅ Minimally invasive
- ✅ Autologous and biocompatible
- ✅ No risk of rejection
- ✅ Outpatient procedure
- ✅ Strong safety profile
- Graph or infographic showing pain improvement over time after PRP injection.
🆚 PRP vs. Traditional Treatments
| Conventional Orthopedic Care | PRP Therapy |
| Corticosteroid injections | Temporary pain relief, no regeneration |
| NSAIDs | Symptom control only |
| Surgery | Invasive, long recovery |
| PRP Therapy | Biological healing, long-term benefit, minimal downtime |
In many cases, PRP can delay or even avoid surgery, especially in early to moderate degenerative conditions.
👨⚕️ Ideal Candidates for PRP Therapy
- Active individuals with tendon, ligament, or joint pain
- Patients with early to moderate osteoarthritis
- Athletes seeking faster recovery and non-surgical solutions
- Patients who did not improve with conventional therapies
⚠️ Not ideal for:
- Severe bone-on-bone arthritis
- Patients on anticoagulation or platelet disorders (case-dependent)
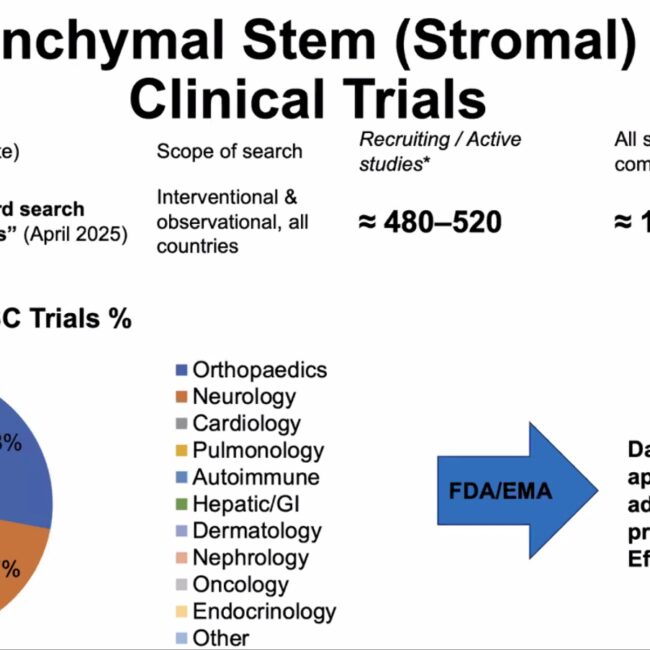
🧠 The Future of Orthobiology
PRP therapy is part of a larger regenerative strategy. The future of orthobiology includes:
- PRP + Stem Cells — synergistic biologic effect
- Exosomes — cell-free biologics for powerful signaling
- Scaffold & biomaterials — to enhance tissue regeneration
- AI-guided personalized treatment protocols
Orthobiology will continue to bridge the gap between conservative care and surgery, redefining orthopedic treatment strategies.
- Futuristic illustration of orthobiologic lab + injection.
📚 References
- Filardo G. et al. Platelet-rich plasma intra-articular knee injections for the treatment of degenerative cartilage lesions and osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2012.
- Mishra A. et al. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med. 2014.
- Samara E. et al. Ultrasound-guided intra-articular injection of expanded umbilical cord MSC with PRP in knee OA.Regen Med. 2022.
- Jo C.H. et al. PRP with MSC injection for rotator cuff disease. Stem Cells. 2018.
If you’re experiencing joint, tendon, or ligament pain, orthobiologic treatments like PRP therapy can help restore function naturally — without surgery.
👉 Book your consultation today