KNEE PAIN ON REGENERATIVE MEDICINE
🦵 Knee Osteoarthritis Treated with Stem Cells: A Breakthrough in Regenerative Medicine
🌿 Introduction: A New Hope for Painful Knees
Knee osteoarthritis (OA) is one of the most common causes of chronic joint pain and mobility loss worldwide. It affects millions of people, particularly those over 40, athletes, or individuals with prior knee injuries.
Conventional treatments — such as painkillers, corticosteroid injections, or even surgery — often focus on symptom relief but do not address the underlying degeneration of cartilage.
Today, regenerative medicine offers a powerful alternative:
👉 Stem cell therapy, a minimally invasive treatment that stimulates the body’s natural healing mechanisms to repair damaged cartilage, reduce inflammation, and restore function.
- Anatomical illustration of the knee joint showing healthy vs osteoarthritic cartilage.
🦴 What Happens in Knee Osteoarthritis?
Knee OA is a degenerative joint disease characterized by:
- Progressive loss of articular cartilage
- Inflammation of the joint lining (synovitis)
- Bone spur formation (osteophytes)
- Pain, stiffness, swelling, and reduced mobility
As cartilage wears away, bones rub against each other, causing pain and mechanical symptoms.
🔸 Traditional treatments (painkillers, hyaluronic acid injections, physical therapy) may provide temporary relief but do not regenerate the cartilage.
🔸 Joint replacement surgery may be necessary in advanced stages — but it is major surgery with a long recovery period.
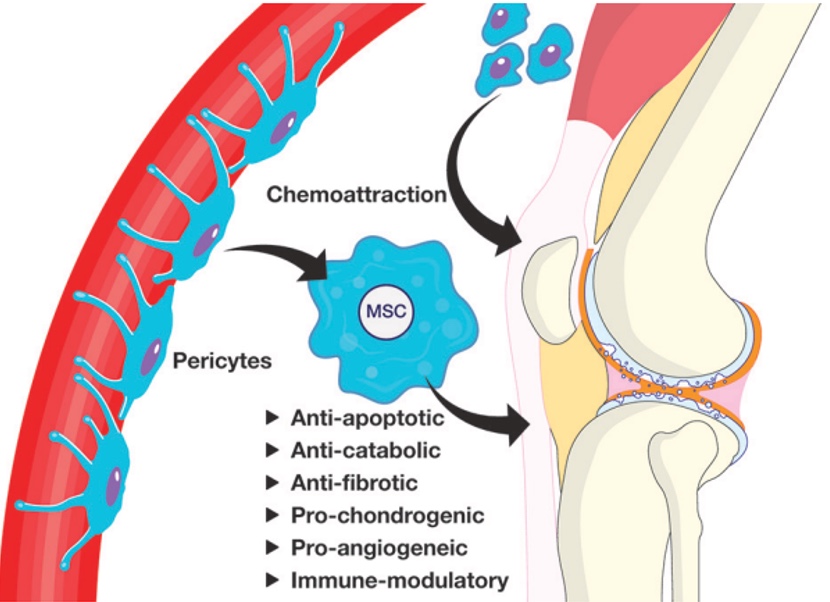
🧬 How Stem Cell Therapy Works in Knee Osteoarthritis
Stem cells are undifferentiated cells capable of becoming specialized cells — including chondrocytes, the cells that make up cartilage.
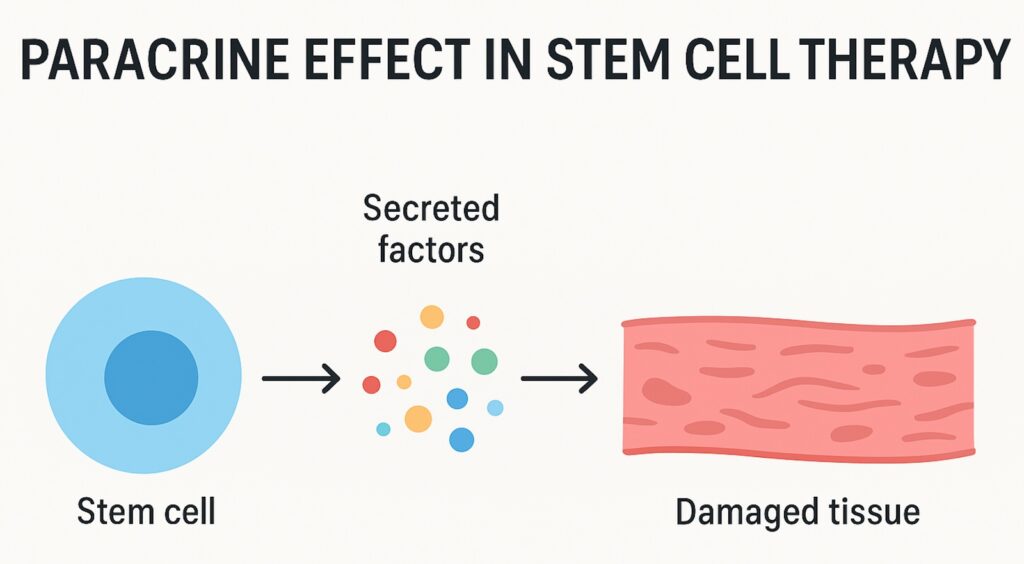
Mechanism of action:
- Anti-inflammatory effect – stem cells reduce joint inflammation.
- Paracrine signaling – they release growth factors and cytokines to stimulate local repair.
- Cartilage regeneration – they can support the repair of worn cartilage.
- Pain modulation – by improving the joint environment, pain and swelling decrease.
- Infographic showing injection of stem cells into the knee and biological response.
🩺 Types of Stem Cells Used in Knee OA Treatment
| Source | Description | Key Benefits |
| Bone marrow (BMSCs) | Harvested from the iliac crest (pelvis) | Autologous, strong regenerative potential |
| Adipose tissue (ADRCs) | Taken from abdominal fat | Abundant, minimally invasive, rich in MSCs |
| Umbilical cord (UC-MSCs) | Allogenic (donor), processed under GMP | High quality, ready-to-use, potent anti-inflammatory effect |
| PRP (Platelet-Rich Plasma) | Platelet concentrate (not stem cells) | Often combined with MSCs to enhance effect |
👉 Umbilical cord MSCs have shown excellent results in published studies, offering a safe and standardized option for patients.
💉 What the Procedure Involves
- Consultation & Imaging
Diagnosis is confirmed using clinical examination and MRI to assess cartilage status. - Cell Preparation
Depending on the protocol, cells are either harvested (autologous) or prepared from donor cord tissue (allogenic). - Ultrasound-Guided Injection
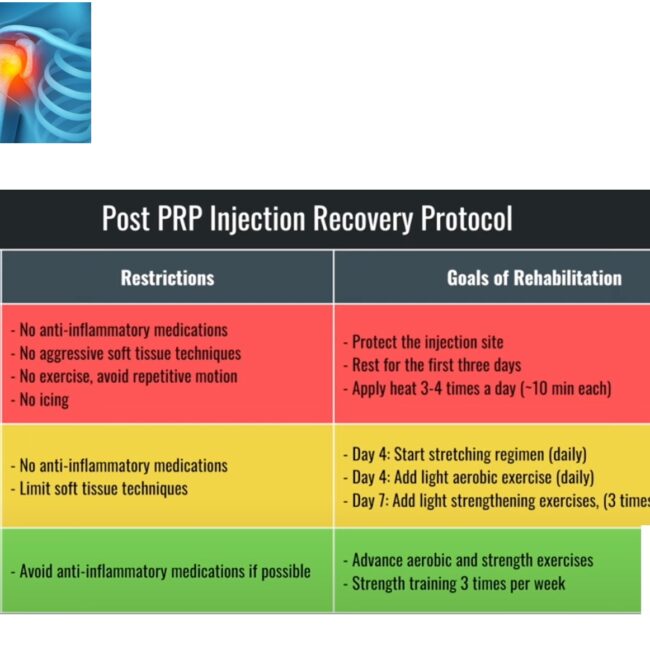
The stem cells are precisely injected into the affected knee joint. - Recovery & Rehabilitation
Patients usually walk the same day. Light activity resumes quickly, and improvement is often noticed within weeks to months.
- Clinical photo or illustration of ultrasound-guided intra-articular knee injection.
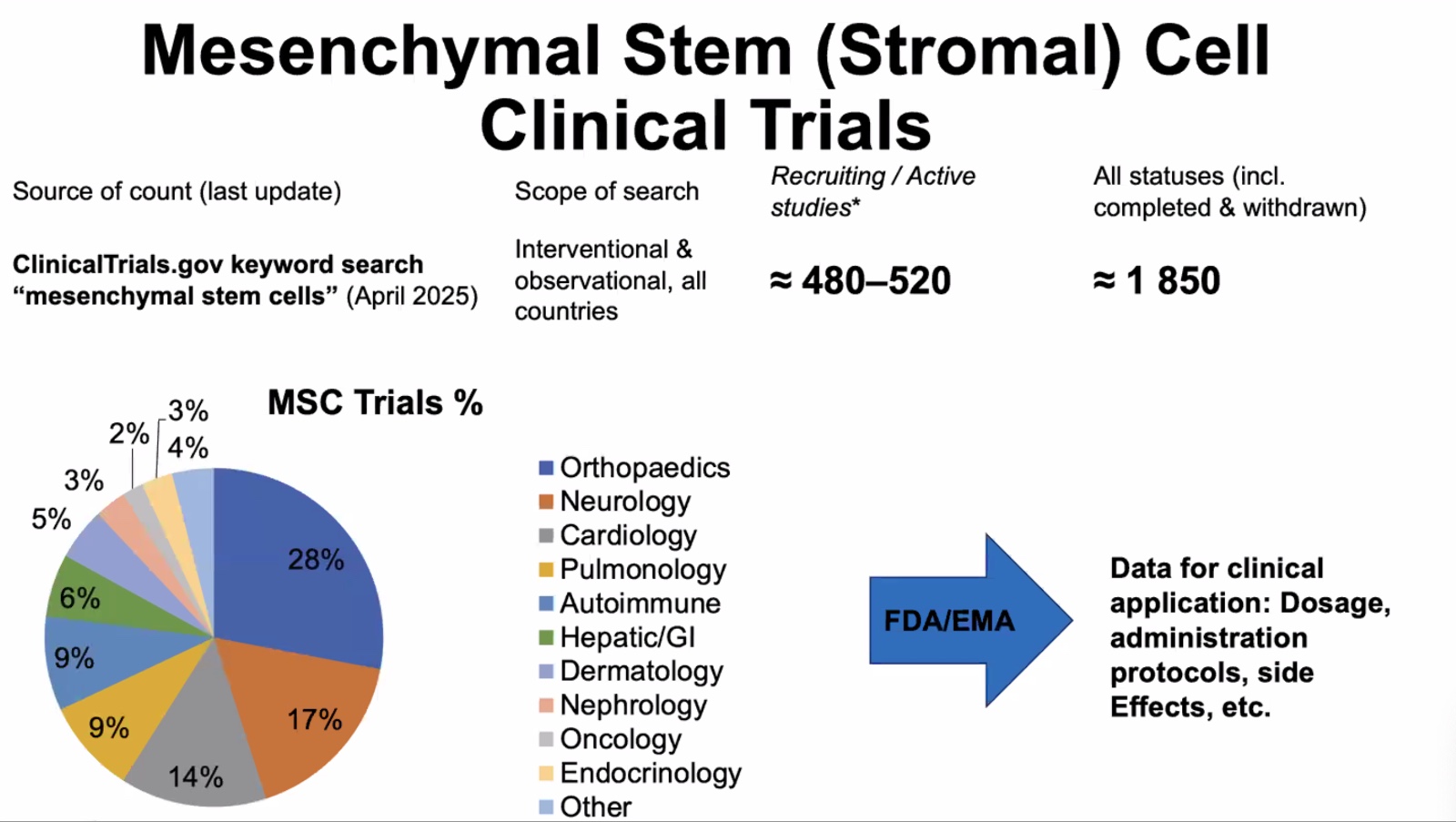
🧪 Scientific Evidence Supporting Stem Cell Therapy in Knee OA
Multiple clinical studies have shown promising outcomes:
- Wang et al., 2016 — Umbilical cord MSC injection led to significant pain reduction and improved function in patients with degenerative knee OA.
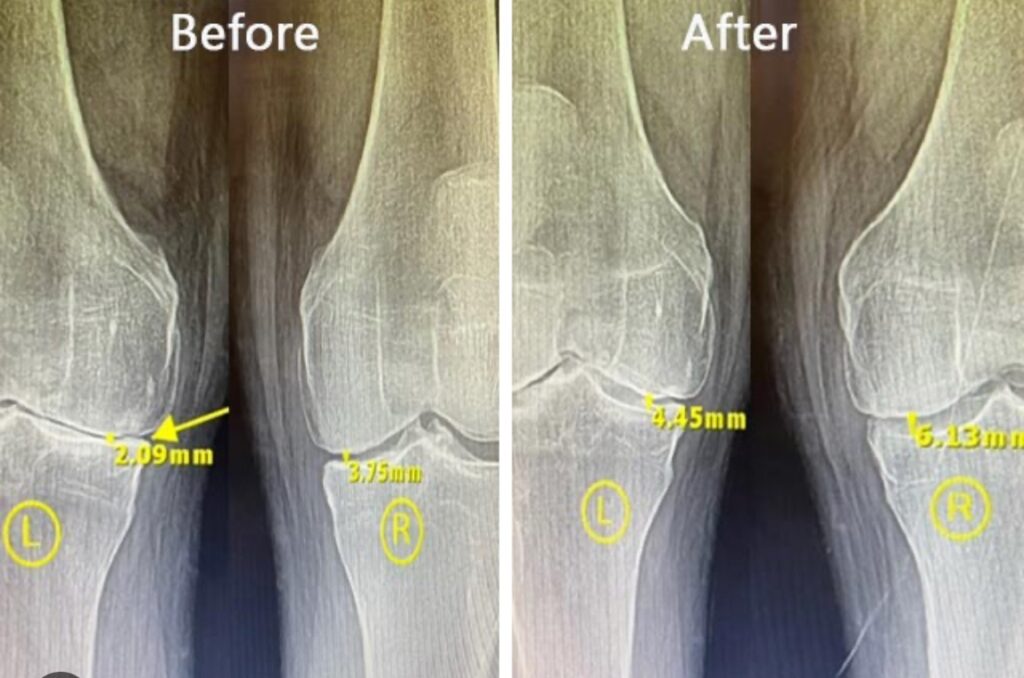
- Samara et al., 2022 — MRI confirmed cartilage regeneration following UC-MSC injection in moderate OA.
- Jo et al., 2018 — Adipose-derived MSCs improved joint function and symptoms in early OA patients.
Reported benefits:
- ✅ Reduced knee pain and swelling
- ✅ Improved walking and daily activities
- ✅ Better cartilage quality in imaging studies
- ✅ Delayed or avoided joint replacement surgery
⚖️ Stem Cell Therapy vs Conventional Treatments
| Conventional Treatment | Stem Cell Therapy |
| Focus on symptom relief | Targets the biological cause |
| Temporary benefit | Long-term cartilage protection |
| Often leads to surgery | May delay or prevent surgery |
| Limited regenerative effect | Promotes natural tissue repair |
👨⚕️ Who Is a Good Candidate?
Stem cell therapy may be suitable for:
- Patients with mild to moderate osteoarthritis
- Those who wish to avoid or delay joint replacement
- Active adults and athletes with cartilage wear
- Individuals who have not responded to conventional treatments
❗ For patients with advanced “bone-on-bone” arthritis, surgical options like total knee replacement may still be needed.
🧭 What to Expect After the Procedure
- Most patients return to daily activity quickly.
- Improvement typically occurs over 2–6 months as tissue remodeling takes place.
- No hospitalization or general anesthesia required.
- Low risk of complications when performed by experienced physicians in certified facilities.
🧠 The Future of Knee OA Treatment
Regenerative medicine is evolving rapidly.
Emerging innovations include:
- Exosomes and biologics for enhanced healing signals
- Gene-edited stem cells for more robust regeneration
- AI-driven patient selection to predict outcomes
- 3D bioprinting for cartilage reconstruction in advanced cases
- Futuristic illustration of cartilage tissue engineering.
📚 References
- Wang L. et al. Curative effect of human umbilical cord mesenchymal stem cells by intra-articular injection for degenerative knee osteoarthritis. 2016.
- Samara E. et al. Ultrasound-guided intra-articular injection of expanded umbilical cord MSCs in knee OA. Regen Med. 2022.
- Jo C.H. et al. Intradermal injection of autologous adipose-derived MSCs for rotator cuff disease. Stem Cells. 2018.
- Caplan A.I., Mesenchymal Stem Cells: Time to Change the Name! Stem Cells Transl Med. 2017.
If you suffer from knee pain or early osteoarthritis, stem cell therapy may help restore your mobility and reduce pain — without surgery.
👉 Book your consultation today