Tendinopathy: Types, Causes, Diagnosis & Management
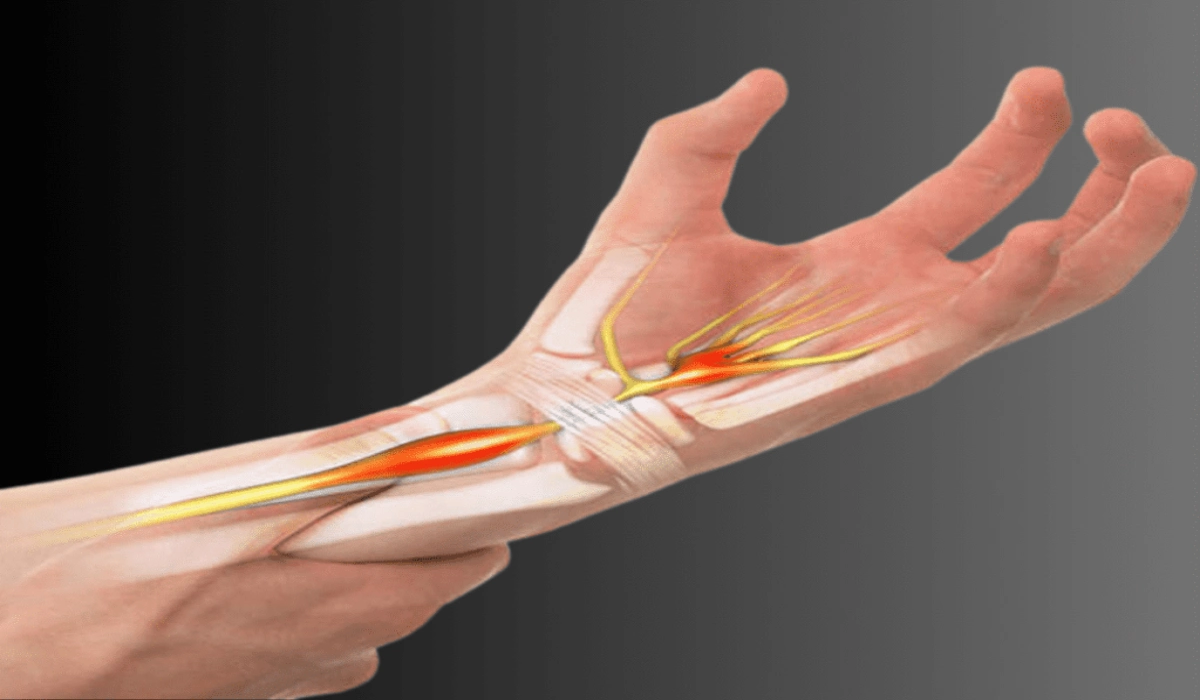
Tendinopathy refers to a group of conditions affecting the tendons, which are the strong, fibrous tissues connecting muscles to bones. It can cause pain, stiffness, and reduced mobility, often interfering with daily tasks or athletic performance.
Tendinopathy develops gradually and is usually linked to overuse, improper movement, or degenerative changes in the tendon. While many people try to manage the condition on their own, proper diagnosis and targeted treatment are essential for long-term recovery.
Why Tendinopathy Deserves More Attention
Tendon problems are common across all age groups. Whether it’s an office worker with an aching elbow or a gym-goer experiencing shoulder discomfort, tendinopathy is often the underlying cause.
In a fast-paced city like Dubai, where residents balance demanding jobs with active lifestyles, tendinopathy is frequently overlooked until symptoms become persistent. Addressing it early can prevent chronic pain and functional limitations.
Understanding Tendinopathy
Tendinopathy is a broad term used to describe tendon disorders, typically involving pain, swelling, and impaired performance. It is often caused by repetitive stress that leads to microtears in the tendon fibres.
Contrary to earlier beliefs, tendinopathy is not primarily an inflammatory condition. Instead, it is marked by degenerative changes in the tendon structure, which is why anti-inflammatory medications may not always be effective.
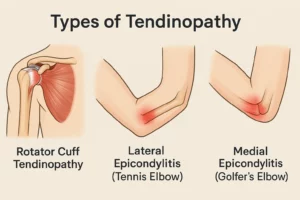
Types of Tendinopathy
Different tendons in the body can be affected, and each presents with slightly different symptoms. The most common types of tendinopathy include:
-
Rotator Cuff Tendinopathy
Affects the shoulder tendons, typically due to repetitive overhead motion. Common in swimmers, tennis players, and those with poor posture.
-
Lateral Epicondylitis (Tennis Elbow)
Pain on the outer part of the elbow caused by overuse of the forearm muscles. Can affect both athletes and office workers.
-
Medial Epicondylitis (Golfer’s Elbow)
Similar to tennis elbow but affects the inner part of the elbow.
Each type varies in presentation but shares a common mechanism involving tendon overload and breakdown.
Causes of Tendinopathy
Several factors contribute to tendon degeneration. The most common causes of tendinopathy include:
Overuse or Repetitive Strain
The most common cause is repeated stress without sufficient rest or recovery time. This leads to small tears and gradual tendon breakdown.
Poor Biomechanics
Misaligned joints or poor technique during movement can place abnormal strain on tendons.
Muscle Imbalance or Weakness
Weak surrounding muscles force the tendon to absorb more load than it should.
Age-Related Changes
As people age, tendons lose elasticity and become more prone to injury.
Medical Conditions
Diabetes, rheumatoid arthritis, and certain medications like corticosteroids or fluoroquinolone antibiotics have been linked to tendon problems.
Recognising the Symptoms
Tendinopathy symptoms can vary depending on the location but often include:
- Pain and tenderness near the affected joint
- Stiffness, especially in the morning or after rest
- Swelling or thickening of the tendon
- Pain that worsens with activity and eases with rest
- Decreased strength or function in the affected area
In the early stages, the pain may come and go. Without treatment, it often becomes persistent and may limit movement or performance.
Diagnosing Tendinopathy
Diagnosis begins with a thorough history and physical examination by a musculoskeletal specialist. The goal is to assess movement patterns, pain triggers, and the specific tendon involved.
Imaging Tests May Include:
- Ultrasound to check for structural changes in the tendon
- MRI to confirm tendon degeneration or rule out tears
- X-rays may be used to rule out bone involvement or arthritis
Accurate diagnosis helps tailor treatment to the stage and severity of the condition.
Managing Tendinopathy
Management of tendinopathy involves relieving symptoms while encouraging tendon healing and strengthening. Treatment plans vary based on the type and severity of the condition.
Activity Modification
Reducing or modifying aggravating activities is often the first step. Complete rest is rarely recommended, as tendons need controlled loading to heal.
Physiotherapy
Rehabilitation focuses on improving flexibility, posture, and strength. Eccentric loading exercises, where the tendon is lengthened under load, have shown excellent results in tendon recovery.
Shockwave Therapy
This non-invasive treatment uses sound waves to stimulate blood flow and promote tendon repair. It may be considered for chronic cases.
Dry Needling
Some specialists use dry needling or tendon fenestration to promote a healing response in the affected area.
Medications
Pain relief may be provided through paracetamol or topical treatments. Anti-inflammatories are sometimes used in early stages, but they do not address the underlying tendon changes.
Injections
Platelet-rich plasma (PRP) injections are gaining popularity for chronic tendinopathy. They involve injecting the patient’s own growth-factor-rich blood components into the affected tendon.
Surgery
Surgical intervention is rare and only considered when all conservative options fail. The goal is to remove degenerated tissue and stimulate healing.
Preventing Tendinopathy
Tendinopathy can often be prevented or its recurrence reduced by following these principles:
- Warm up properly before physical activity
- Avoid sudden increases in exercise intensity
- Focus on technique and posture during movement
- Strengthen muscles around the joint to reduce load on tendons
- Incorporate regular stretching and mobility work
- Listen to the body and rest if early signs of tendon strain appear
These strategies are particularly important for athletes, older adults, and people with a history of tendon problems.
Frequently Asked Questions
Is tendinopathy the same as tendinitis?
Not exactly. Tendinitis refers to inflammation, while tendinopathy refers to the degenerative changes that occur over time. Most chronic tendon problems are actually tendinopathies.
How long does tendinopathy take to heal?
Recovery time varies depending on severity. Mild cases may improve in a few weeks, while chronic conditions can take several months.
Can tendinopathy heal without treatment?
It is possible for mild cases, but proper treatment ensures a more complete recovery and reduces the risk of recurrence.
Should I stop exercising completely?
No, controlled movement and gradual loading are essential for recovery. Avoiding painful activities is advised, but physiotherapist-guided exercise is usually part of the plan.
When should medical help be sought?
If pain persists for more than two weeks, interferes with function, or worsens over time, it is important to consult a specialist.
Doctor’s Note
Tendinopathy is a treatable condition, but it often requires patience and a structured plan. Early diagnosis, targeted rehabilitation, and consistent follow-through are the key components of successful recovery. Individuals with recurring symptoms should be assessed for underlying mechanical or systemic factors.
Conclusion
If you are experiencing persistent joint or tendon pain that affects your mobility or performance, it may be a sign of tendinopathy. Early consultation can prevent long-term complications and speed up recovery. Dr. Marouane, Consultant Orthopaedic Specialist in Dubai, offers comprehensive care for all types of tendinopathy with advanced, evidence-based treatment options.